- 15% of the world’s population (1.1 billion people) had a mental illness in 2016.
- It is expected that 45% of us will experience a mental illness in our lifetimes.
- 1 in 5 Australians are currently suffering from a mental illness.
- 1 in 4 people aged 55+ on psychiatric medications.
- Current treatment options are inadequate: typical treatments work for only about 30-35% of people with mental illness, and even when they do, most continue to experience some symptoms, and most relapse within the first year or two after treatment stops.
- In Australia, mental illness is the leading cause of non-fatal disease burden, and the third leading cause of total disease burden.
- The direct cost of mental illness in Australia is at least $60 billion annually with indirect costs amounting to $180 billion annually, prior to the Covid-19 pandemic.
- Well-designed clinical trials with psychedelic-assisted psychotherapy have produced impressive results, demonstrating their potential to be a game-changer for mental health treatment.
Get real with the current state of mental health in Australia and around the world
To illustrate the magnitude of the issues that Mind Medicine Australia aims to help address, we present some basic numbers relevant to mental illness in Australia, and globally. Mental illness refers to clinically diagnosable psychological, emotional, or behavioural ‘disorders’, for example, depression, anxiety, substance use, and post-traumatic stress disorder. These disorders can vary in severity and duration, and often have damaging effects not only on the afflicted individual, but on their families and peers, with far-reaching consequences for society as a whole.
Global mental illness – prevalence and burden
An estimated 15% of the world’s population (a staggering 1.1 billion people) had a mental illness in 2016[i]. Currently, over 300 million people suffer with depressive disorder, equivalent to 4.4% of the world’s population[ii]. Regions with the highest rates of mental illness globally include Australia, North America, and Western Europe (see Figure 1). A number of explanations for this pattern have been put forward (for example, see Whitaker[iii])
Across all diseases, five types of mental illness appeared in the top 20 causes of global disease burden in 2013 (which takes into account both death and disability)[iv]. Globally, mental illness has been estimated to account for over 7% (ranked 5th) of the global disease burden, though some argue this is a gross underestimation[v]. Depression is ranked by WHO as the single largest contributor to non-fatal global disability (7.5% of all years lived with disability in 2015); anxiety disorders are ranked 6th (3.4%)[ii].
Share of population with mental health and substance use disorders, 2016
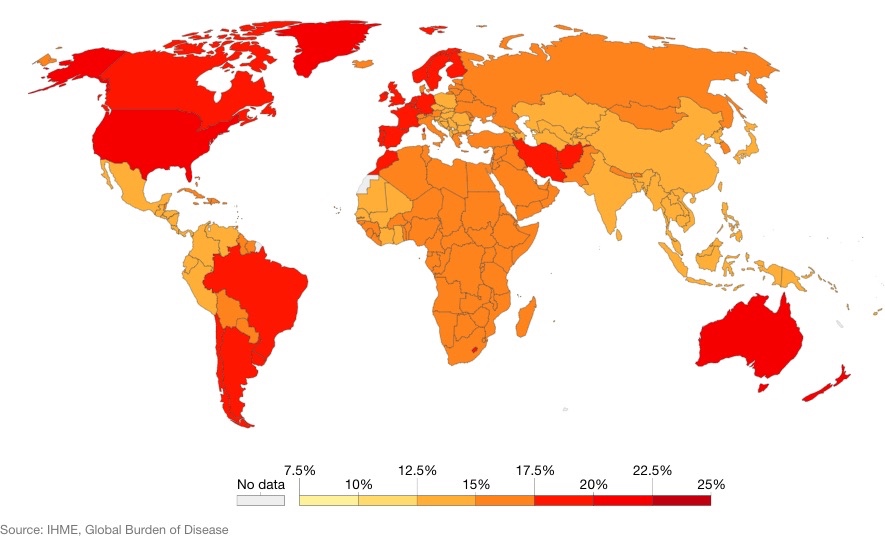
FIGURE 1: Share of population with any mental health or substance use disorder; this includes depression, anxiety, bipolar, eating disorders, alcohol or drug use disorders, and schizophrenia. Due to the widespread under-diagnosis, these estimates use a combination of sources, including medical and national records, epidemiological data, survey data, and meta-regression models. Hannah Ritchie and Max Roser (2019) – “Mental Health”. Published online at OurWorldInData.org. Retrieved from: ‘https://ourworldindata.org/mental-health’
Australia mental illness – prevalence and burden
In 2017-18, one in five (4.8 million) Australians aged 16 to 85 had a current and chronic mental health or behavioural condition[vi]. This number has been steadily increasing, up nearly 3% from the 2014-15 National Health Survey. At least 45%[vii] of Australians will experience a mental illness in their lifetime[viii].
The most common mental illnesses in Australia are depression, anxiety, and substance use disorders (often occurring together). In a single year, 13% of Australians will be diagnosed with an anxiety-related condition (e.g., post-traumatic stress disorder, social phobia), 10% with a depression-related condition[vi], and over 5% of Australian adults generally[ix], and 13% of people aged 16-24, will be diagnosed with a substance use disorder[x]. Diagnoses aside, in 2017-18, 13% (2.4 million) of Australians reported high or very high levels of psychosocial distress over the past 4 weeks alone[vi].
Mental illness in Australia – Harms
In 2011, mental illness was responsible for 12% of the total disease burden in Australia (years of life lost and years of life lived with disability, combined), behind only cancer and cardiovascular disease[xi]. When considering only years lived with disability (non-fatal disease burden), mental illness was the leading cause.
An estimated 200 Australians attempt to take their life each day[xii], and the suicide rate in Australia has been steadily on the rise over the past decade. Suicide is the 13th leading cause of death – over 3,000 Australians take their life each year, or 8-9 people each day[xiii]. The more prevalent causes of death are attributable to factors largely associated with old age, with median ages of death for these causes typically in the 80s – the median age for suicide is 45 years. Mood disorders (including depression and anxiety) are the leading cause of suicide, accounting for 43% of Australian suicides in 2017-18[xiii].
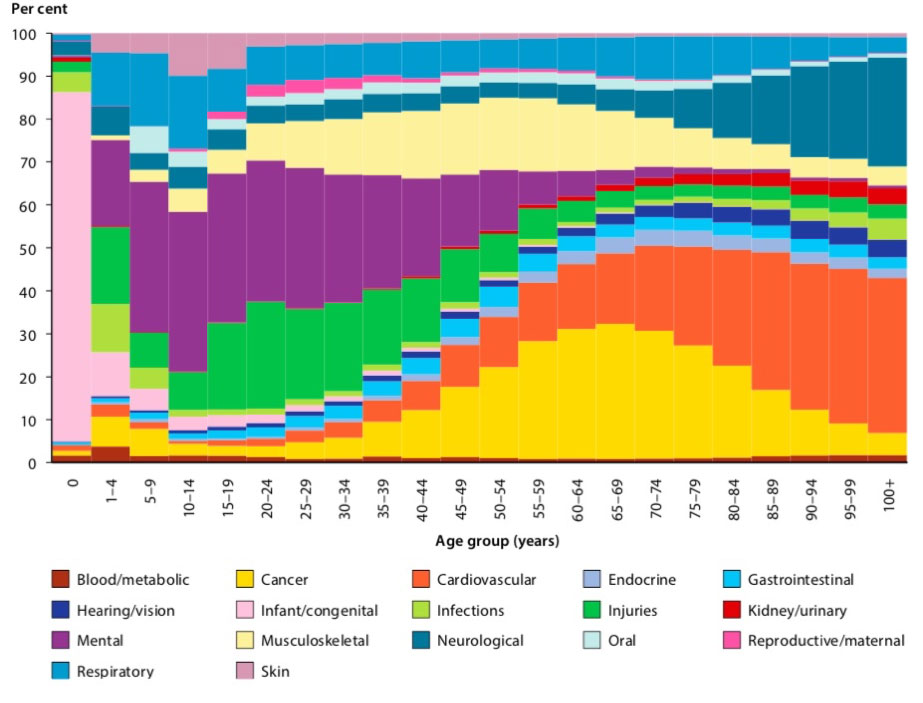
FIGURE 2: Relative proportion of total burden (DALY), by disease group and age, 2011 AIHW (Australian Institute of Health and Welfare) 2016. Australian Burden of Disease Study: impact and causes of illness and death in Australia 2011. Australian Burden of Disease Study series no. 3. Cat. No. BOD 4. Canberra: AIHW.
Mental Illness in Australia – Costs
In 2017-18, Australians aged 15-64 with a mental or behavioural illness were nearly twice as likely to be unemployed or not in the labour force (37.8%) than those without such an illness (20.5%). A 2013 report commissioned by Medibank and Nous Group found the overall cost of supporting people with a mental illness to be at least $28.6 billion annually, far exceeding previous estimates that failed to consider numerous non-health expenses (e.g., income support, housing, criminal justice)[xiv]. This estimate, which does not include indirect costs such as lost productivity, amounts to 2.2% of Australia’s Gross Domestic Product (see Figure 3).
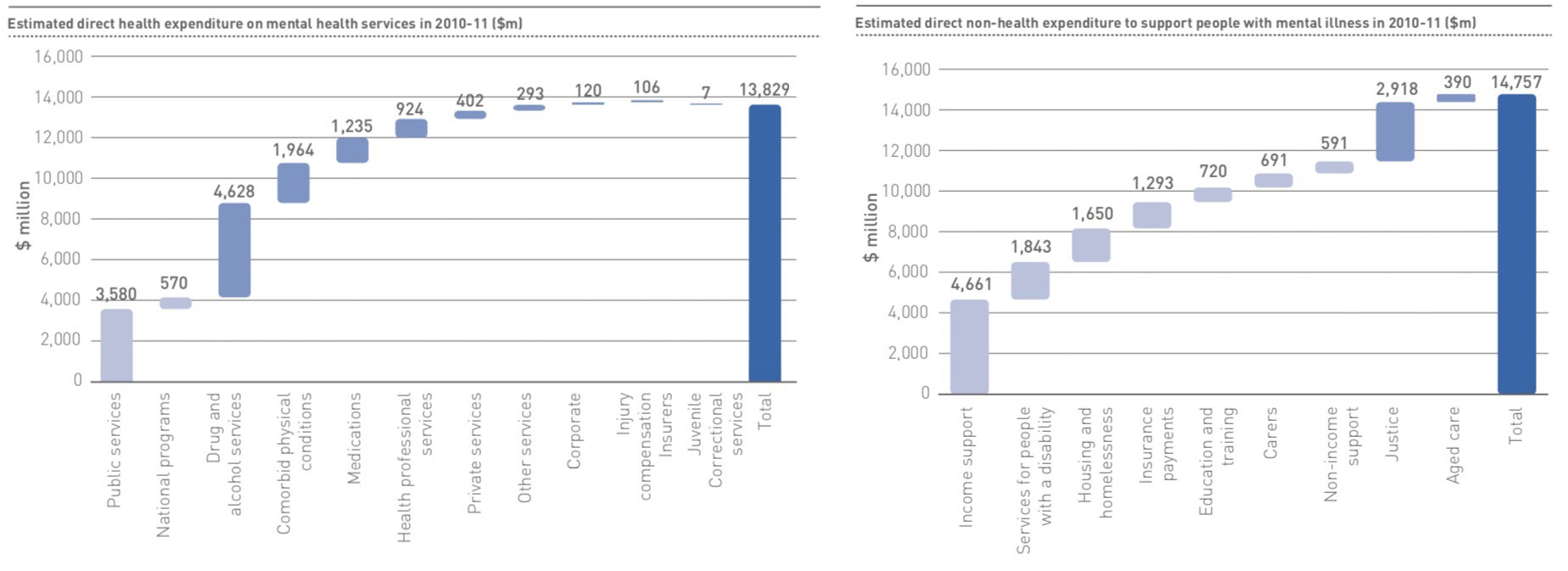
FIGURE 3: Direct health-related and direct non-health-related expenditure on mental illness in Australia, 2013. Medibank Private Limited and Nous Group. (2013). The Case for Mental Health Reform in Australia: A Review of Expenditure and System Design.
Mental Illness in Australia – Pandemic
- “A new joint report by Mission Australia and Black Dog Institute reveals that substantially more young people in Australia are experiencing psychological distress than in 2012. The report also reveals that young people had higher odds of experiencing psychological distress if they identified as female, non-binary, living with disability, or as Aboriginal or Torres Strait Islander. One in four young people in 2020 said they are experiencing mental health challenges; a significant increase since 2012 when one in five young people were facing similar concerns.” Read more.
- “Mental health service ReachOut has released a new report which provides vital insights into the mental health of young people living in regional, rural and remote (rural) areas across Australia, tracked over a five year period.* The report includes indications that the mental health of young people in these areas is worsening, alongside more positive findings such as that rural young peoples’ mental health literacy is improving.” Read more.
- A new study published in the Lancet on 8 October 2021 documents a world-wide increase of more than 129 million cases of major depression (53.2mn) and anxiety (76.2mn) disorders during the pandemic. The authors attribute this to the combined effects of the pandemic and lockdown measures.
- United Nations: We need to take action to address the mental health crisis in this pandemic. “Even without the pandemic, one in four of us will suffer a mental health episode during our lifetimes. The shocks associated with COVID-19 are now pushing many towards greater fragility and pain: grief at the loss of loved ones; anxiety at the loss of jobs; isolation and restrictions on movement; difficult family dynamics; uncertainty and fear for the future. Each of these on its own can trigger or deepen distress. Today many people are suffering several simultaneously.” Read the full article here.
Mental Illness Treatment
Under 50% of Australians with a mental illness will access mental health services in a given 12-month period[xv]. For those who do, outcomes are typically far from satisfactory. In spite of a vast global effort to understand and treat mental illness – notwithstanding the development of a few treatments that have helped a minority of sufferers in a sustainable way – the effectiveness of treatment remains inadequate. For example, only 40 to 60% of depressed individuals respond to current chemical or talk therapies[xvi], with the majority experiencing ongoing symptoms that fall below diagnostic thresholds, and between 50% and 80% relapse when treatment stops[xvii,xviii,xxi,xx]. In addition, psychotherapy is often associated with high economic costs, and chemical therapies are usually associated with considerable side-effects.
In this context of high prevalence, debilitating cost to human life and society, and inadequate treatment outcomes following decades of global research, new approaches are urgently needed. Psychedelic-assisted psychotherapies are poised to usher in a new era in mental health treatment.
Psychedelic-Assisted Psychotherapy
To date, psychedelic-assisted psychotherapy research is showing strong clinical results, and is beginning to receive limited regulatory approval in healthcare systems globally.
Click here for information about psychedelic assisted therapies.
Further Information
For further information on research and therapy using psychedelic-assisted therapies, read our literature review.
For a list of some current and past research in this space we suggest our knowledge page and this list of research from The Multidisciplinary Association for Psychedelic Studies (MAPS).
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016
- Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO.
- Whitaker, R. (2010). Anatomy of an Epidemic: Magic Bullets. Psychiatric Drugs, and the Astonishing Rise of Mental Illness in America New York: Crown Publishers.
- Vos, T., Barber, R. M., Bell, B., Bertozzi-Villa, A., Biryukov, S., Bolliger, I., … & Duan, L. (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 386(9995), 743-800.
- Vigo, D., Thornicroft, G., & Atun, R. (2016). Estimating the true global burden of mental illness. The Lancet Psychiatry, 3(2), 171-178.
- Australian Bureau of Statistics 2018, National Health Survey First Results, cat. no. 4364.0.55.001, ABS, Canberra.
- A likely underestimation due to it being reported over 10 years ago.
- Australian Bureau of Statistics. (2009). National Survey of Mental Health and Wellbeing: Summary of Results, 4326.0, 2007. ABS: Canberra.
- Australian Bureau of Statistics 2007, National Survey of Mental Health and Wellbeing: Summary of Results, cat. no. 4326.0, ABS, Canberra.
- AIHW (Australian Institute of Health and Welfare) 2011. Young Australians: their health and wellbeing 2011. Cat. no. PHE 140 Canberra: AIHW
- AIHW (Australian Institute of Health and Welfare) 2016. Australian Burden of Disease Study: impact and causes of illness and death in Australia 2011. Australian Burden of Disease Study series no. 3. Cat. No. BOD 4. Canberra: AIHW.
- The Australian Senate. (2010). The Hidden Toll: Suicide in Australia Report of the Senate Community Affairs References Committee. Commonwealth of Australia, Canberra.
- Australian Bureau of Statistics 2017, Causes of Death, Australia, cat. no. 3303.0, ABS, Canberra.
- Medibank Private Limited and Nous Group. (2013). The Case for Mental Health Reform in Australia: A Review of Expenditure and System Design.
- Whiteford HA, Buckingham WJ, Harris MG, Burgess PM, Pirkis JE, Barendregt JJ and Hall WD 2014. Estimating treatment rates for mental disorders in Australia. Australian Health Review 38(1):80–5
- APA. (2000). Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Revised (DSM-IV-TR). Washington, DC: American Psychiatric Publishing.
- Belsher, G., & Costello, C. G. (1988). Relapse after recovery from unipolar depression: a critical review. Psychological bulletin, 104(1), 84.
- Hollon, S. D., Thase, M. E., & Markowitz, J. C. (2002). Treatment and prevention of depression. Psychological Science in the Public Interest, 3(2), 39-77.
- Judd, L. L. (1997). The clinical course of unipolar major depressive disorders. Archives of General Psychiatry, 54(11), 989.
- Mueller, T. I., Leon, A. C., Keller, M. B., Solomon, D. A., Endicott, J., Coryell, W., . . . Maser, J. D. (1999). Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. American Journal of Psychiatry, 156(7), 1000-1006.
