
In recent years, psychedelic-assisted therapies have emerged as a promising approach for individuals living with treatment-resistant mental health conditions. Australia has become a key player in this evolving field, particularly following a landmark regulatory decision in early 2023. That year, the Therapeutic Goods Administration (TGA) rescheduled psilocybin and MDMA as Schedule 8 medicines, allowing their limited use in treating certain mental illnesses. This change followed applications submitted by Mind Medicine Australia —an organisation that played a central role in supporting the rescheduling through formal submissions, public education, and expert engagement. It marked a world-first in regulatory recognition of these substances for therapeutic use.
Since then, a growing number of authorised psychiatrists in Australia have begun offering these therapies under the TGA’s Authorised Prescriber scheme. As of early 2024, more than 110+ patients have received psychedelic-assisted therapy in regulated clinical settings—marking a significant turning point in mental healthcare delivery.
Current mental health treatments are not always effective. In Australia, one in five people experiences a mental illness each year, and around half of those do not find relief through conventional approaches such as antidepressants or talk therapy. For individuals with treatment-resistant depression or PTSD, this can mean years of ongoing symptoms with few alternatives.
Psychedelic-assisted therapies are now being studied and applied as potential new options. Rather than solely addressing symptoms, these therapies aim to support deeper psychological processing through a structured process that includes professional guidance and preparation.
Psychedelic-assisted therapy typically combines the administration of a psychedelic substance—such as psilocybin, MDMA, or ketamine—with a multi-phase therapeutic process:
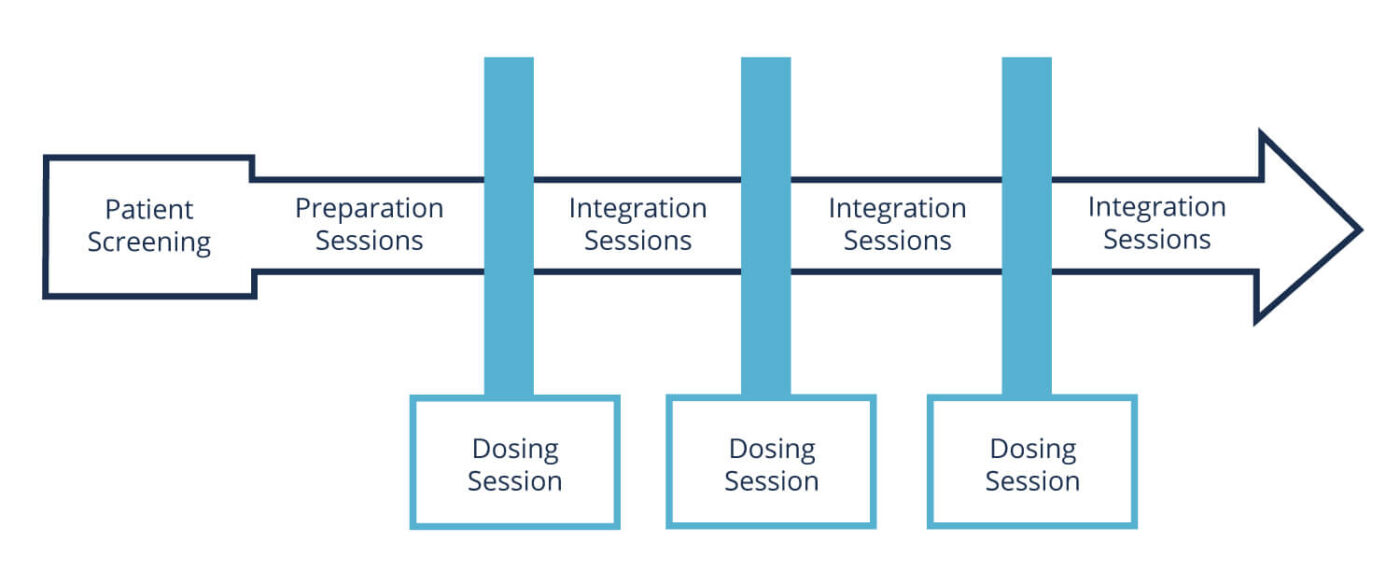
Participants are screened carefully, and sessions are delivered with support from trained professionals to ensure safety and therapeutic value.
Each substance works differently: for example, psilocybin has been associated with increased neuroplasticity and emotional openness, while MDMA reduces fear responses and may support trauma-focused work. Ketamine, already used in psychiatry, can have rapid-acting antidepressant effects in some individuals.
As the field grows, appropriate training for healthcare professionals has become increasingly important. The Certificate in Psychedelic-Assisted Therapies (CPAT)™ by Mind Medicine Australia is one such initiative. The program is designed to provide registered clinicians—such as psychiatrists, psychologists, GPs, nurses, and allied health professionals—with a foundation in the theory and practice of psychedelic-assisted therapy.
The training combines online learning with in-person components and is delivered by an international faculty of clinicians and researchers. It covers the clinical application of psilocybin, MDMA, and ketamine-assisted therapy, with attention to ethics, trauma-informed care, and best practices for safety and integration. By the end of 2025, the program is expected to have trained over 600 professionals across Australia.
Programs like CPAT aim to prepare mental health professionals to work safely within the current regulatory environment and to support multidisciplinary models of care.
Growing international research supports the therapeutic potential of psychedelic-assisted therapies. Studies conducted at institutions such as Johns Hopkins University and Imperial College London have found that one to three sessions can lead to significant reductions in symptoms for people with depression, PTSD, anxiety, and end-of-life distress. Some trials report remission rates of 60–80% in populations that had not responded to other treatments.
Neuroimaging studies have also shown that psychedelics can temporarily alter patterns of brain activity associated with rigid thinking, while enhancing communication between brain regions—potentially contributing to psychological flexibility and new insights.
The reintroduction of psychedelic-assisted therapies into clinical settings brings with it a range of ethical, regulatory, and professional questions. As the field develops, further research, training, and careful oversight will be essential to ensure these therapies are delivered responsibly.
With the support of frameworks like the TGA’s Authorised Prescriber scheme and professional training programs such as CPAT, Australia is entering a new chapter in mental healthcare—one that is shaped by both scientific inquiry and clinical need.
Disclaimer: This article is for educational purposes only and does not constitute medical advice. Psychedelic-assisted therapies are available in Australia only through authorised prescribers under the TGA framework. Please consult a qualified health professional before considering any treatment options.