In our first six years, we have made remarkable progress in growing public awareness of and creating access pathways for Psychedelic-Assisted Therapies in Australia. With the success of our rescheduling applications in early 2023, we are now seeing patients being treated with psilocybin and MDMA-assisted therapies for treatment-resistant depression and PTSD respectively. This is an important and historic moment for these therapies and for mental health treatment in Australia.
The TGA decision provides access to these innovative treatments for Australians suffering from treatment-resistant mental illness and paves the way to treat other illnesses such as addictions, obsessive-compulsive disorder, anorexia, cognitive decline and end-of-life stress in the future. In January 2024, the first patients were treated with psychedelic-assisted therapies in Melbourne, Australia. These were the first psychedelic medicine dosing sessions in clinical settings in 50 years. We estimate that 80 patients received psychedelic-assisted psychotherapy in Australia in 2024. We project that this number will increase dramatically in 2025 as the number of psychiatrists authorised to deliver PAT continues to increase.
Our goal is to build the ecosystem for these treatments in Australia. Everyone meeting the medical criteria should be able to access psychedelic-assisted therapies in medically controlled environments. Please see our key strategic objectives below.

What we have achieved in six years with your support:
Awareness and Knowledge Building
• 230+ webinars including FREE Global Webinar Series with the leaders in the field, numerous documentary screenings and a range of special events attracting 42,000+ participants
• Facilitating Professor David Nutt’s incredibly successful Australian tour in November 2022, where he presented to public audiences, clinicians and decision makers. This tour included a presentation to over 130 people at the TGA in relation to the rescheduling of MDMA and psilocybin.
• Launch of free online Global Webinar Series where World-leading experts provide illuminating presentations and conversations about the ground-breaking opportunity psychedelic-assisted therapies offer and other related topics.
• Launch of Mind Medicine Australia Podcast series featuring 56 podcasts with leaders in psychedelics
• Launch of MMA Weekly Meditation Sessions
• Video animation explaining the mental illness epidemic in Australia and the benefits of psilocybin and MDMA-assisted psychotherapy with 80,000+ views
• Created a short documentary, Science vs Stigma, to dispel some of the myths associated with these important medicines with over 29,000+ views
• Over 155,000+ views of Shroom Boom, a light-hearted music video
• Implemented a Board Observership program in conjunction with VMIAC
• Appointed as Member of peak body, Mental Health Australia
• Launch of MMA online shop selling a range of unique merchandise including Australia’s first book of Psychedelic Healing Stories
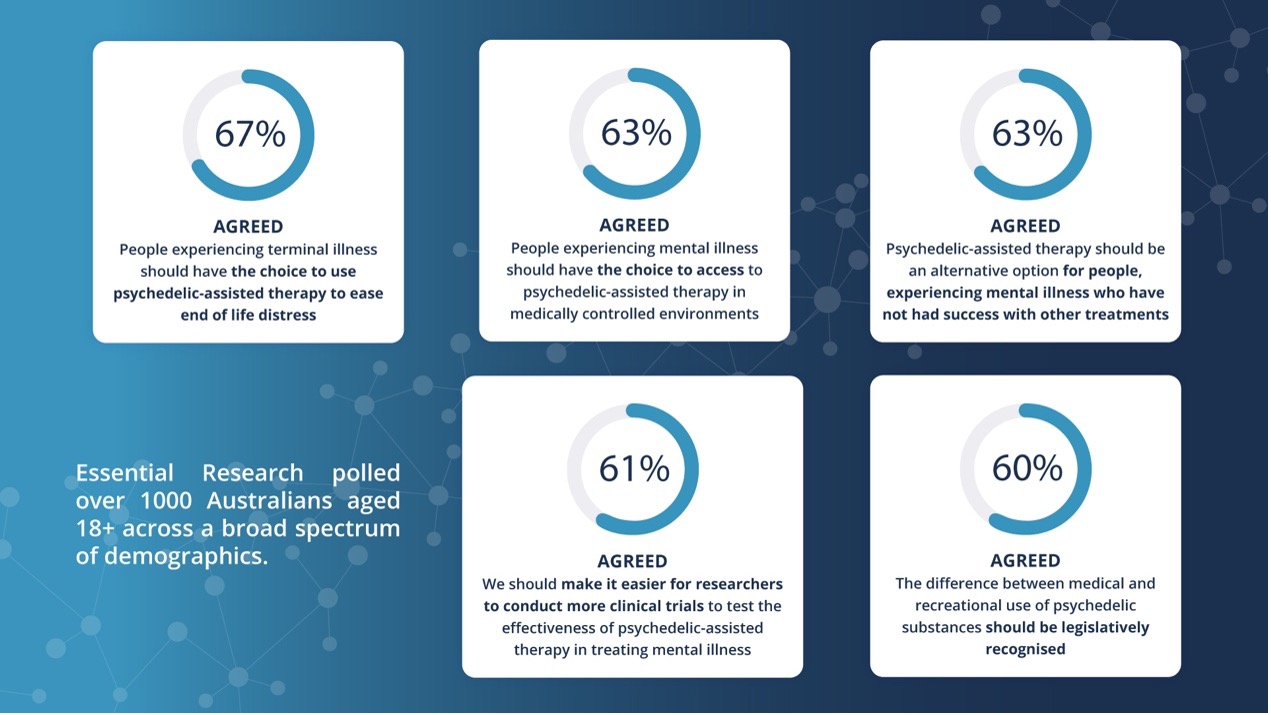
• Initiated Australia’s first Essential Research poll to gauge the sentiment of the Australian public on the issue of access to psychedelic medicines in medically controlled environments as treatments for key classes of mental illness. 67% agreed that ‘People experiencing terminal illness should have the choice to use psychedelic-assisted therapies to ease end of life distress’.
• Developed summary of all trials taking place in Australia
• Over 705,000+ visits to the Mind Medicine Australia website
• Over 101,700+ followers on our social media channels
• Over 684,000+ views on our YouTube Channel and 5371+ subscribers
• Over 11,000+ visits to our e-book about psychedelic-assisted psychotherapies
• An engaged database of over 72,000+ diverse people from a range of sectors and 47,000+ people on our mailing list
• 680+ donors
• 310+ media appearances across Australia’s biggest publications including national news
• 33+ local Chapters around Australia and New Zealand with 2200+ members and growing
• 55,000+ views to our TGA How-to guide during the 2022 public submission period
• Presented and produced Mind Medicine Australia’s inaugural International Summit on Psychedelic Therapies for Mental Illness in November 2021
• Nearly 1000 people registered for our two-day workshop and Global Summit from every state of Australia and more than 15 other nations
• Over 90,000 views of our Summit sizzle reel
• Over 80,000 visits to the Summit website
• Over 5000 queries received from the Summit website
• 110 virtual breakout rooms
• 32 global leaders in the field presented on a range of topics
• 19 major Corporate partners
• Over 160 Education partners
• 17 Supplier Partners
• 15 Media Partners
• 8 Scholarship winners
• 5 Poster winners
• 1 global 4-day event with massive impact
Patient Access
• Successful submissions made to the TGA to reschedule MDMA and psilocybin from Schedule 9 (Prohibited Substances) to Schedule 8 (Controlled Medicines), allowing limited access to MDMA and psilocybin-assisted therapies from July 1 2023 via the TGA’s Authorised Prescriber scheme
• Granted an Innovation Patent over an improved method of synthesis of MDMA
• Successfully procured medical grade GMP standard MDMA and psilocybin for import to Australia for use in trials and as part of the TGA’s Authorised Prescriber scheme from July 1 2023. We provide equitable access to GMP quality medicine as an exclusive distributor in Australia for Optimi Health
• In January 2024, the first patients were treated with psychedelic-assisted therapies as part of the Therapeutic Goods Administration’s (TGA) Authorised Prescriber (AP) program in Melbourne, Australia with medicines and training supplied through Mind Medicine Australia. These were the first psychedelic medicine dosing sessions in clinical settings in 50 years.
• Established the Patient Support Fund (PSF). Donations into this fund provide subsidised treatment for those who otherwise could not afford it. We have supported 9 patients with a total commitment of $85.000+ in its first year.
• Collaborating with Health Insurers and Governments to broaden the funding base for these therapies
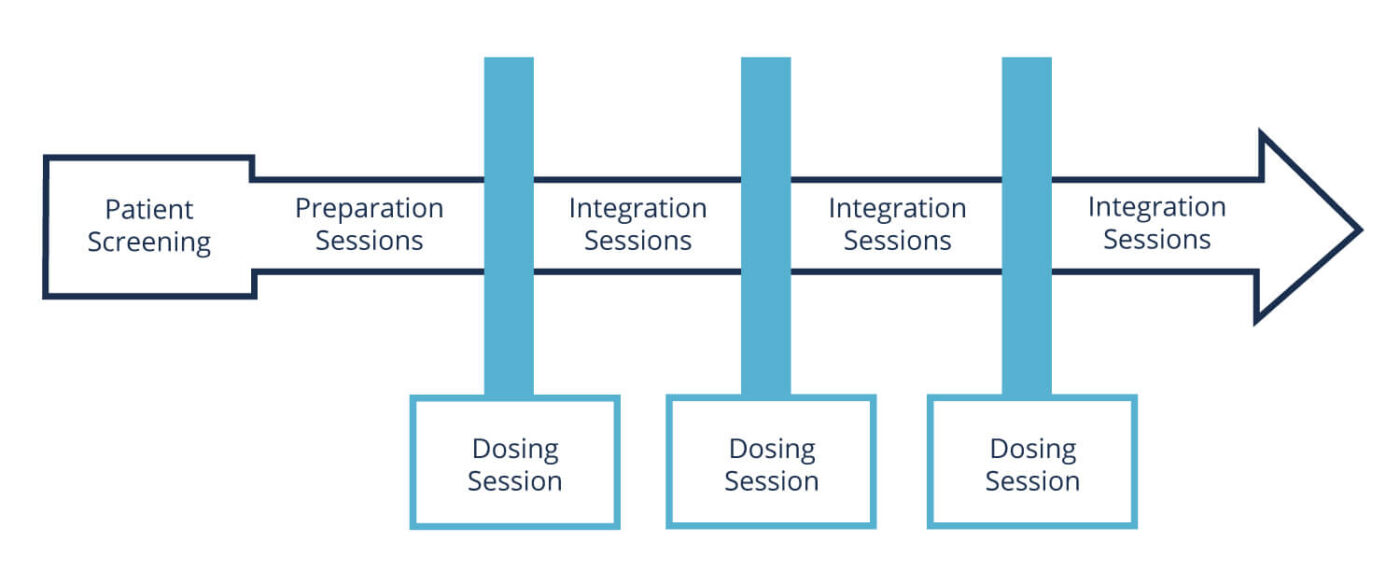
• Developing a gold standard National Care Program, clinical protocols and standard operating practices for psychedelic-assisted therapies in partnership with leading clinical groups around Australia
Professional Development Program
• Our highly anticipated Certificate in Psychedelic-Assisted Therapies commenced in January 2021 featuring a world class Faculty. By the end of 2024, there will be over 500 qualified therapists including psychiatrists, GPs, physicians, psychologists, psychotherapists counsellors, nurses, social workers, occupational therapists, addiction specialists, paramedics and other allied health professionals.
• Confirmed world-leading facilitators for our Certificate in Psychedelic-Assisted Therapies (CPAT) professional development course
• Engaged Dr Gita Vaid (USA) as the course’s International Course Director and Dr Eli Kotler as the Australian Course Director for our programs from 2023 onwards.
• Described as “the best course of its kind in the world” by Professor David Nutt on ABC Radio National interview (UK)
• Over 1000+ applications received since launch
• Over 1333+ people trained in psychedelic-assisted therapies across our suite of training programs
• Over $434,000 raised for CPAT grants through philanthropy to support those in regional and rural areas and therapists suffering financial hardship. Over 85 grants have been awarded so far.
• Over 183,000+ views of the CPAT highlights sizzle reels. Watch current reel.
• Launch of the Fundamentals in Psychedelic-Assisted Therapies Course
• Developed a mentoring program for graduates of PAT training, allowing ongoing professional development with global leaders in the field
• Recognition by key peak/membership bodies of our professional development and training programs
• Key university student placement partnerships with University of Melbourne and a major volunteering program established
Research
• Successfully advocated for $15 million to support innovative mental health clinical trials utilising psychedelic-assisted therapies from the Federal Government through the Medical Research Futures Fund
• Supported the launch of Psychedelic-Assisted therapies Research Registry at ANU, which will allow for outcome data to be collected from treatment with PAT around Australia
• Launch of The Monash University Neuromedicines Discovery Centre, initially proposed by MMA and developed over a 2-year period
• 32+ current trials of psilocybin, MDMA, LSD and Ibogaine in Australia and New Zealand.
• Developed a BLOG, significant education resources and partnered with Universities to disseminate these as well as sharing these via our website
• Discussions with key University stakeholders continue
• Mind Medicine Australia, Marks 5-Year Milestone with Global Achievements in Psychedelic Therapies
• Psychiatrists give the First Psychedelic Medicine Dosing Sessions in Clinical Settings in 50 Years this Week in Melbourne Australia
• Breaking News: The TGA Announces the Delegate’s Final Decision to Reschedule the Use of Psilocybin and MDMA for Medical Purposes
• An Open Letter to the Prime Minister in November 2022
• TGA Expert Review Findings Support the Therapeutic Use of Medicinal Psychedelics in Treating Mental Health Crisis in October 2021
• Mind Medicine Australia Launched Australia’s First Book of Psychedelic Healing Stories in October 2021
• Monash University announced the establishment of the Neuromedicines Discovery Centre to Focus on Psychedelic-Assisted Therapies for the Treatment of Key Classes of Mental Illness in November 2021
• Mind Medicine Australia hosted Australia’s Inaugural International Summit on Psychedelic Therapies for Mental Illness online in November 2021
• Mind Medicine Australia joined a global coalition launched to secure a rescheduling of psilocybin under the 1971 UN Convention on Psychotropic Substances in January 2022
• New Polling by Mind Medicine Australia Revealed Over 60% of Australians Support Increased Access to Psychedelic Medicines in February 2022
• Mind Medicine Australia Lodged New Applications for the Restricted Medical use of MDMA and Psilocybin Assisted Therapies for Patients with Treatment Resistant Mental Illnesses in March 2022. The full applications can be found here.
The progress we are making in public education was exemplified in several headline media articles including in the Australian Financial Review, The Australian, The Age, Herald Sun, The Saturday Paper and Vogue Australia and media interviews including with Channel Nine, Channel 10, The Project, ABC and numerous other TV and radio stations and online media.
In February 2023 the TGA announced that MMA’s rescheduling applications for MDMA and psilocybin were successful. This decision allows psychiatrists to apply for Authorised Prescriber status to administer psilocybin-assisted therapy for treatment-resistant depression and MDMA-assisted therapy for PTSD.
Our primary focus over the next couple of years will be on facilitating the roll out of psilocybin and MDMA-assisted psychotherapy in light of this regulatory change. We are also interested in novel research in this rapidly emerging field to treat a variety of conditions.
Behind the scenes, we are working closely with key stakeholders to ensure that these therapies will be accessible and affordable to all Australians needing these treatments in medically controlled environments, so that cost and geography doesn’t become a barrier.
In the last six years, we have assembled a comprehensive leadership team with expertise in mental illness including psychology, neuroscience and pharmacology, non-profit development, business practices and networks, public health, events, marketing and educational development.
Mind Medicine Australia is also supported by an outstanding Board, Ambassadors, and an Advisory Panel of over 70 local and international experts in medicine, psychiatry, psychology, pharmacology, research, science more broadly, ethics, law, policy, anthropology, business and therapeutic practices. We have also developed a Lived Experience and Young Leaders Panel.
As we move through 2024, our vision and capacity continue to grow. With these medicines now legally available in Australia on a restricted basis, we turn our focus toward ensuring they are accessible and affordable to all Australians who meet the medical criteria.
We ask for your continued and expanded support so that we can fund the path for psilocybin and MDMA-assisted psychotherapy to help treat the millions experiencing key mental illnesses in Australia. This is personal for every one of us.
As Carl Jung said, “The sole purpose of human existence is to kindle a light in the darkness of mere being.”
With gratitude for your interest and generosity. There has never been a more important time to support innovation in the treatment of mental illness.
Peter Hunt AM and Tania de Jong AM