The life and legacy of the late, great Augustus Owsley Stanley III. Why he was a key figure in the 1960’s counterculture movement, and responsible for ultimately altering the collective consciousness of a generation.
The tropical Cairns of Far North Queensland is the last place you’d expect to see someone with such celebratory status as Owsley Stanley. Yet, this is where he’d chosen to live for the last two decades of his life. A climate change refugee, Australia became his home after he predicted that the northern hemisphere would be ruined by uncontrollable storms causing a new ice-age. It was here he died, a citizen of the country, in a car accident in March 2011.
Owsley Stanley neighboured with the untouched vastness of the Daintree rainforest, the oldest rainforest in the world — which is where our journey begins. Likewise, this is too where I called home for the past year of my life. A music and psychedelic enthusiast myself, my path and Owsley’s met when I had the great pleasure of meeting and speaking to his daughter Redbird Ferguson, who is also Chief Financial Officer of the Owsley Stanley Foundation.
The more I learnt about Owsley Stanley’s life, the more I realised why we have him to thank for paving part of the way for the psychedelic resurgence. His legacy only validates and unveils the unique psychedelic tapestry that links creativity and culture. His story reflects the connection between the psychedelic experience and its impact on human consciousness and cognition in ways that influence innovation, scientific inquiry, and philosophical exploration.
EARLY LIFE
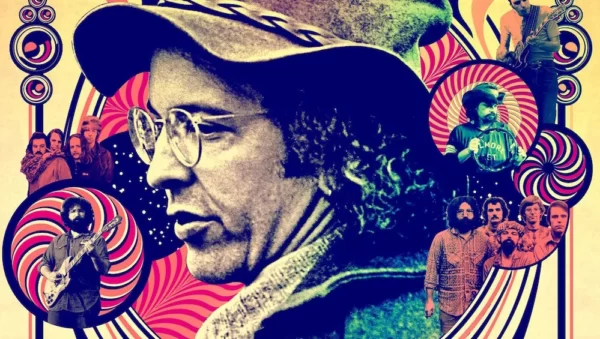
Known to many under his life-long nickname ‘Bear’, the pioneering sound man for the Grateful Dead was born in 1935. His father was a prominent government attorney, and his grandfather was elected as Governor of Kentucky in 1919. Even without graduating high school, he was admitted to the University of Virginia, where he studied engineering for a year. Although he eventually dropped out of college, his lack of formal education didn’t hinder him. Bear ultimately secured a position in the United States Air Force in 1956 as an electronics specialist, serving for 18 months.
He was first introduced to psychedelics when he was enrolled at the University of California, Berkeley for a semester in 1963. After consuming the original Sandoz LSD, he became determined to learn how to synthesise it himself. Using his Berkeley lab, he ordered 500 grams of lysergic acid monohydrate, the basis for LSD, which was legal at the time. Bear went on to perfect and produce a staggering 300,000 doses of LSD in his home laboratory.
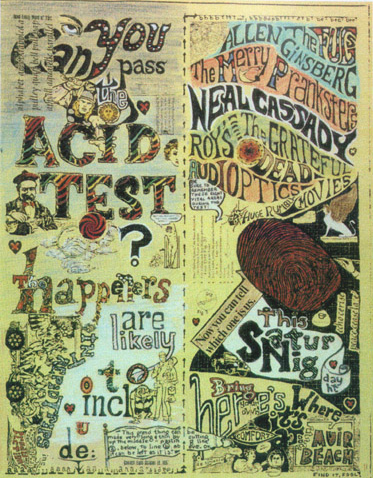
THE ACID TESTS
It was Bear’s acid behind the infamous ‘Acid Tests’ conducted by the novelist Ken Kesey and his Merry Pranksters, the group of psychedelic devotees. The tests were essentially a series of parties held during the mid 1960’s. They comprised of musical performances along with strobe lights, fluorescent paint and of course, LSD. The Acid Tests are notable for their influence on the counterculture of the San Francisco area and subsequent transition from the beat generation to the hippie movement. As bands such as the Dead played, the audience drank Kool-Aid laced with LSD.
Bear eventually used the money he generated selling acid to help fund the early days of the Grateful Dead. Guitarist Jimi Hendrix sampled his product, as did the Rolling Stones’ Brian Jones, Pete Townshend of The Who, Jefferson Airplane, Frank Zappa, and The Beatles among others.
John Lennon had apparently developed an appreciation for LSD in England and wanted to obtain enough high-quality acid to fuel his creative endeavours. According to legend, Lennon approached Bear about a lifetime supply. The effects of the Beatles’ psychedelic experiences on Bear’s acid likely contributed to the band’s trippy ‘Magical Mystery Tour’ film. It is said that even Albert Hoffman, the first synthesiser of LSD, was quite impressed with the product Bear created, as he was the only one who had ever got the chemistry correct.
Some people view LSD as the prime catalyst of the hippy counterculture. It couldn’t be confined to research and government-led projects. By 1966, “Turn on, tune in, drop out” was the catchphrase popularised by LSD enthusiast Timothy Leary, who credited Bear for his contribution. In his ‘Sixties anthology of essays, Politics of Ecstasy’ Leary predicted, “The television folk heroes of today are the merry outlaws of the past. The Television Robin hoods of the future, the folk heroes of the twenty-first century, will be the psychedelic drug promoters, A.O.S. 3, acid king, LSD millionaire, test-tube Pancho Villa, is the best-known of a band of dedicated starry-eyed crusaders who outwitted the wicked, gun-toting federals and bravely turned on the land of the young and the free to the electronic harmony of the future.” A.O.S.3. was Leary’s acronymic code for the name that Bear was given at birth — Augustus Owsley Stanley III.
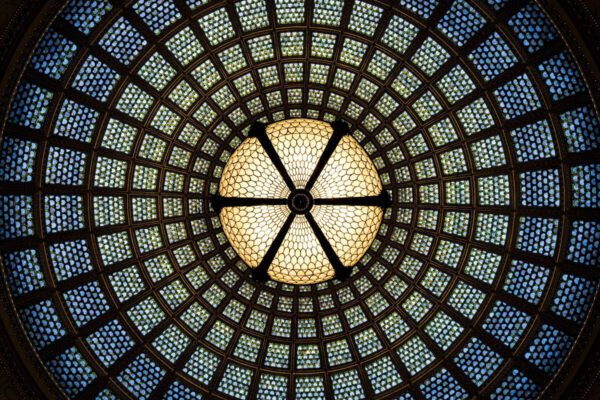
When he wasn’t making the colourful acid tabs known on the street as “White Lightning,” Bear served as the sound engineer for the Grateful Dead. An early and enthusiastic fan, he worked for years to develop the Dead’s “wall of sound,” a 40-foot-tall bank of more than 600 speakers whose output could be controlled by the musicians on stage. This system redefined concert sound reinforcement and set new standards for immersive live experiences. Additionally, he designed the band’s symbol of a lightning bolt inside a skull, known as the “Steal Your Face” logo.
Bear’s use and distribution of high-quality LSD had a significant impact on musicians and their creative processes. Many artists credited LSD with expanding their consciousness and influencing their musical compositions. The psychedelic experience often found its way into the lyrics, sounds, and imagery of the music produced during that era.
BLENDING OF SENSES
“Psychedelics seemed to give me access to my head in some way… I got involved with it because the first time I did it, I realised it opened a door and it was a place I wanted to explore. I wanted to know what I was doing… I guess I’m a good cook. It was the introduction to magic. I’m sure it was the root source of my ability to manipulate sound” (Stanley, 1991).
Bear continued “I was looking at sound coming out of the speakers…” describing an LSD induced trip and added that he’s never met anyone else who’s had the same experience. Interestingly, again this is where Bear and my story intertwines. A high school dropout myself, I eventually went on to study Music at University and too became profoundly transformed by psychedelic revelations. During a psylocibin trip in Joshua Tree, I and the two other women who partook in the ceremony witnessed similar visions to Bear. A phenomenon known as ‘synesthesia’, is where you experience one of your senses through another. For us, it occurred after strumming a guitar and physically seeing the vibrations being fashioned from the strings. The science of how and why this happened fascinates me.

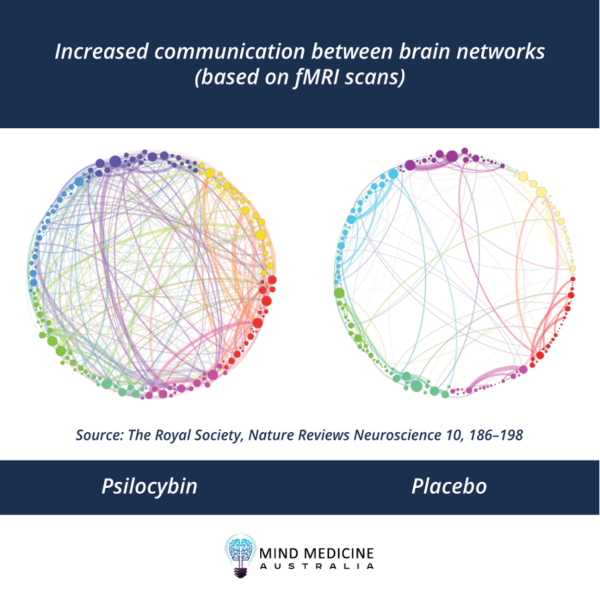
There have now been numerous accounts of synesthesia being experienced during psychedelic trips. With a study being done by David Luke, a London-based researcher at the University of Greenwich. Luke and colleagues found that, a diverse set of drugs can cause synesthesia. LSD and other tryptamines, such as DMT and psilocybin, are more commonly able to induce the phenomenon. These drugs predominantly affect the serotonin systems which aligns with past research suggesting that synesthesia follows a serotonergic pathway. Luke believes research on psychedelic produced synesthesia could be “a back-door way to understand synesthesia,” as 57% of LSD users surveyed experience it.
Luke adds that research about synesthesia can shed light on what neurobiology researchers call the “binding problem.” This is how items that are encoded by distinct brain circuits can be combined for perception, decision, and action. How do humans take different pieces of sensory input that are processed in distinct regions of the brain, such as the motion of a car or the colour red, and bind them cognitively into one coherent perceptual experience? It helps us understand and navigate the world, and it’s a process that’s not yet deeply understood on a neurobiological level. Research on synesthesia and how it relates to the binding problem, may point toward a relationship between psychedelics and human cognition. According to Luke, his work “goes a long way to substantiating or shoring up the stoned ape hypothesis of Terence McKenna… synesthesia induced by psychedelics may have been important in the development of language.”
PSYCHEDELIC AND ALCHEMY INTERTWINE
Another link between psychedelic and human consciousness is one that is more commonly dismissed as a pseudoscience but was frequently referred to by Bear. He was “a savant with an obsession for quality, but his rigor was influenced by spiritual concerns as much as scientific ones” (Jarnow, 2001). “Since LSD itself modulated the mind, Owsley assumed that it was profoundly sensitive to the atmosphere in which it was made, and he approached making it as an alchemical act, with a fanatical concern for purity of both heart and chemistry. His standards were so exacting that he rejected a significant proportion of his yield” (McNally, 2001).
Bear openly spoke about alchemy and psychedelics. These seemingly unrelated realms of human exploration share a captivating connection that spans across time, geography, and cultural contexts. Both fields delve into the depths of transformation and transcendence, whether it be of matter or of consciousness. By recognising these connections, we gain a deeper understanding of the human drive to explore the unknown and to seek transformation in both the external and internal realms.
Alchemy, a mystical and proto-scientific pursuit, emerged in various cultures across the world, from ancient Egypt and Greece to medieval Europe. It aimed to transmute base metals into precious ones and discover the elusive “philosopher’s stone” that held the key to eternal life. Turns out J.K Rowling didn’t pluck Harry Potter from thin air. While on the quest for the stone, alchemists spent a great deal of time studying properties of chemicals and how they interacted. Consequently, alchemy formed the foundation of modern chemistry and medicine.
“Let it be known there is a fountain, that was not made by the hands of men.”
– Ripple, The Grateful Dead
Similarly, indigenous cultures and ancient civilisations have long employed natural substances, often psychedelic plants, or fungi, for spiritual and transformative purposes. Shamans and mystics used these substances to access altered states of consciousness and gain insights into the nature of reality. Both alchemy and psychedelics share an underlying theme of transcendence. Alchemists sought to transform not only physical substances but also their own spiritual selves, embracing the belief that material and spiritual evolution were intertwined. This mirrors the experiences reported by individuals who have undergone psychedelic journeys, often describing a profound shift in their sense of self and connection to the universe. The seven steps of the alchemical process include: calcination, dissolution, separation, conjunction, fermentation, distillation, and coagulation. The parallels between these steps and the psychedelic experience itself is often speculated.
In today’s world, the connection between alchemy and psychotropic experiences continues to intrigue scholars, scientists, and artists alike. As research into the therapeutic potential of psychedelics gains great momentum, similarities are drawn to the alchemical pursuit of transformation and healing. The exploration of the mind’s hidden depths through psychedelics echoes the alchemical quest to unveil hidden truths within matter.
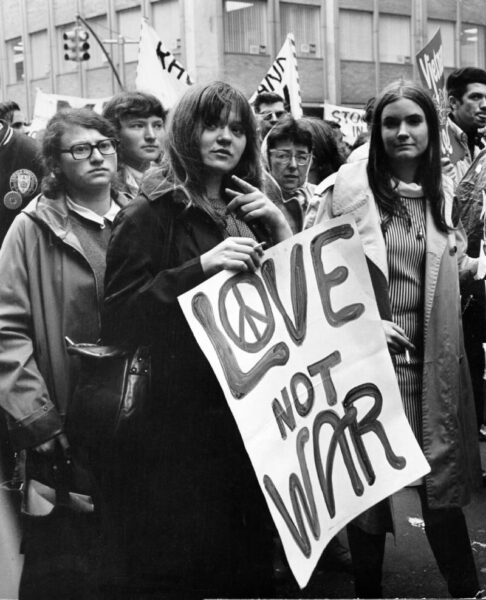
RETURN OF A REVOLUTION
Owsley Stanley was an outlier from birth. Society at the time, perceived him as a threat to the status quo. He rejected the idea of fame, expressing to Rolling Stone magazine “I’m not into being a celebrity, because I think celebrityhood has no value to anyone, least of all the celebrity.” However, in death his fame is still emerging. I believe his story is an important one to tell, as the Summer of Love might have only been an ordinary season without Bear’s pharmaceutical input. It is my objective to shine light on key figures in history that changed the trajectory of our world through the enhancement of their imagination and creativity by psychedelics.
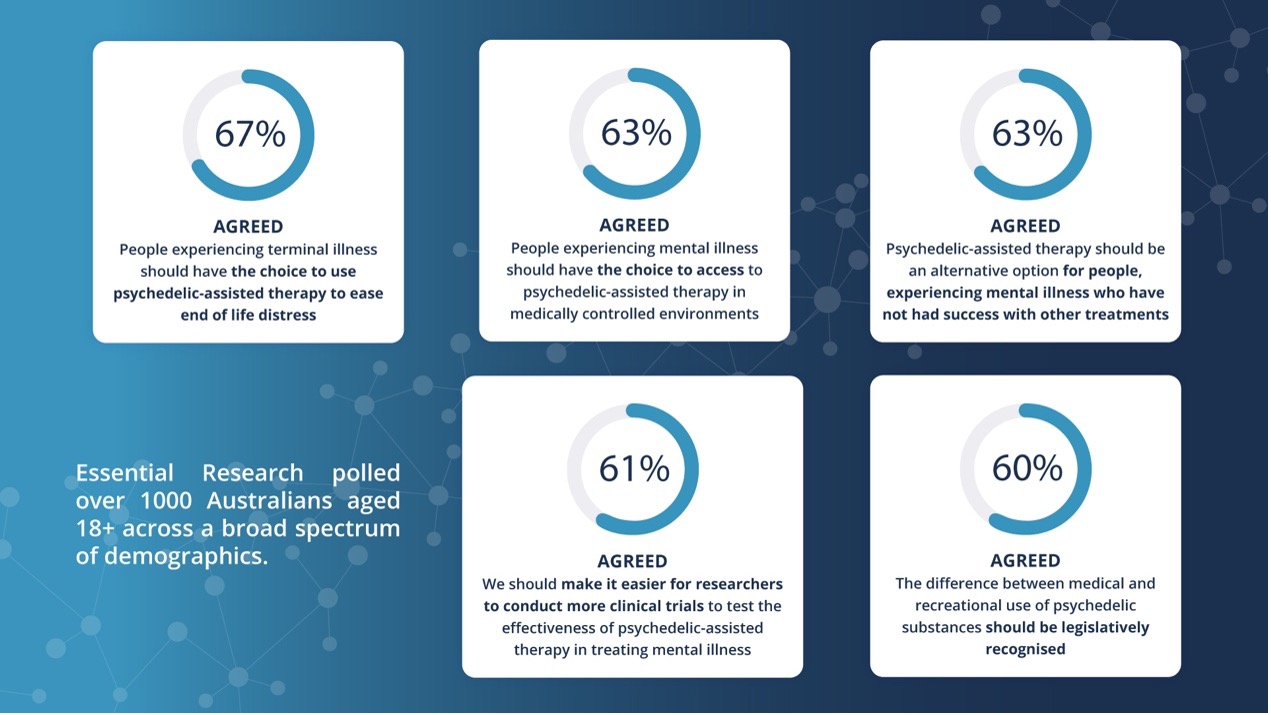
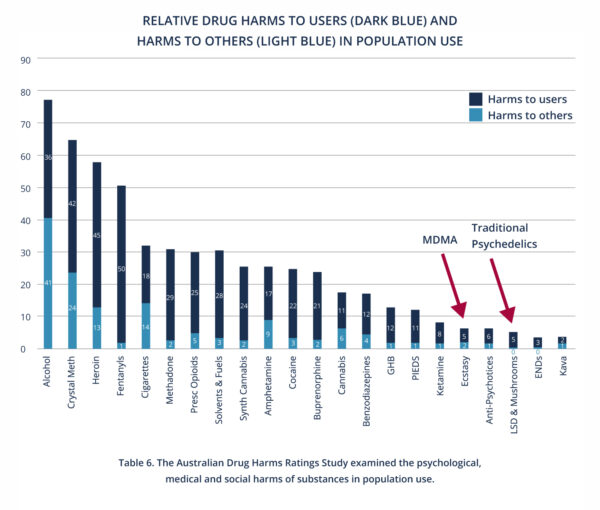
In saying this, we need to be aware of the reasons that the 60’s went sideways. LSD Dose-for-dose tops all other hallucinogens in potency, as other hallucinogens require a much larger dose. Notorious figures such as Timothy Leary and Ken Kesey passed out the drug far and wide to anyone. Even though it was a small amount, it was blowing people out of their minds. Potency is possibly why you don’t see as much research on LSD versus other psychedelics like psilocybin. People need to be mindful of its effects and when and where to indulge. With the therapeutic use of psylocibin and MDMA now legal in Australia, I assume other countries will shortly follow suit. We are being presented with the opportunity to steer psychedelics back on the right path and use them how they should have been intended, as medicine.
I have previously written in articles about the more specific research behind psychedelic medicine, and how it can unlock creativity by quietening the default mode network, consequently creating new thought patterns in the brain. Perhaps the average person may not invent the next million-dollar idea or scientific discovery, but they have the possibility to change their life and in turn fill it with more beauty. This directly influences others around them and the world at large. With that said, in a world heading for environmental crisis, who knows what problems may be solved by having psychedelics in the right hands. As science and spirituality converge, advocates are starting to bridge the gaps and harness the potential of these compounds for societal betterment. As the legalisation of psychedelic-assisted therapy proposes solace to the terminally ill and those suffering with mental health challenges, it too offers insights into the human psyche.
Bear introduced a generation to the power of these medicines. Beyond his direct influence on music production and performances, his innovative spirit inspired a generation of musicians, engineers, and artists. Bear’s emphasis on pushing boundaries and embracing experimentation left a lasting mark on the music industry and continues to influence how music is created today.
As psychedelics start to become reintroduced into society, I trust that the world will begin to remember our ancient history. Psychedelics is the thread that weaves cultures together. We are only starting to unravel the mysteries of alchemy and psychoactive compounds. We now stand at the crossroads of ancient wisdom and cutting-edge science, seeking to unlock the keys to transformation, both within and beyond. So, thank you Bear for your countless contributions, I’m grateful our paths met in a roundabout way. In the words of the Dead, “what a long, strange trip it’s been.”
REFERENCES
Adams, B.M. (2023) The age of Alchemy, High Times. Available at: https://hightimes.com/culture/the-age-of-alchemy/ (Accessed: 28 July 2023).
Bannerman, M. (2019) The man who brought LSD to America invented something else that also changed music forever, ABC News. Available at: https://www.abc.net.au/news/2019-03-24/stanley-owsleys-work-with-1960s-bands-must-be-preserved/10871062 (Accessed: 28 July 2023).
Bears Sonic Journals (2022) Owsley Stanley Foundation. Available at: https://owsleystanleyfoundation.org/ (Accessed: 15 August 2023).
Brown, E. (2023) ‘Bear’ Stanley, who made the LSD on which Haight-Ashbury tripped, dies at 76, The Washington Post. Available at: https://www.washingtonpost.com/local/obituaries/bear-stanley-who-made-the-lsd-on-which-haight-ashbury-tripped-dies-at-76/2011/03/15/ABt95Ib_story.html (Accessed: 12 August 2023).
Cassandra, R. (2022) Psychedelics open opportunity to study synesthesia — lucid news, Lucid News — Psychedelics, Consciousness Technology, and the Future of Wellness. Available at: https://www.lucid.news/psychedelics-open-opportunity-to-study-synesthesia/ (Accessed: 12 August 2023).
Getlen, L. (2016) This guy made the best LSD of the ’60s, New York Post. Available at: https://nypost.com/2016/11/19/this-guy-made-the-best-lsd-of-the-60s/ (Accessed: 15 August 2023).
Kitchens, T. The Johnny Appleseed of LSD (2016) KY for KY Store. Available at: https://kyforky.com/blogs/journal/owsley (Accessed: 12 August 2023).
McNally,Dennis (2002) A long strange trip: The inside history of the Grateful Dead. Broadway Books, NY.
NonDirectionalFilms (2022) OWSLEY STANLEY INTERVIEW. [Online video] Available at: https://www.youtube.com/watch?v=vjWKNw4nKOs (Accessed: 28 July 2023).
Pierce, M. (2023) The alchemical journey: Exploring the parallels with the psychedelic experience, Medium. Available at: https://medium.com/@mikejaypierce/the-alchemical-journey-exploring-the-parallels-with-the-psychedelic-experience-ca7708ccd71d (Accessed: 15 August 2023).
Charlotte McAdam
I am a natural health consultant, globetrotter, music enthusiast and freelance writer specialising in the natural healthcare industry. A psychonaut, who draws from my life story and many experiences with indigenous ceremonies from around the world. I am passionate about the ancient teachings of these medicines and how they can help heal our relationship to ourselves, each other and mother earth.