What is shadow work?
Shadow work is a term coined by Carl Jung, the Swiss Psychoanalyst and close collaborator of Sigmund Freud. It refers to working with all the aspects of the mind that are obscured or hidden from view. When we gaze up into the night sky we are often met by the glow of the moon. We see the brightness and the subtle contours of aspects of the moon’s surface if we look closely enough. We also understand that there is a dark side of the moon, hidden from our view but no less clearly there. In shadow work we are speaking about the dark side of the mind. Not dark in the Judeo-Christian sense of bad or evil, but simply that which isn’t seen. Called variously the unconscious or the subconscious, it is the repository of emotions, experiences, memories, culture, family patterns, all of which are obscured but which also impact on the function of our personality.
In Jungian terms, many psychological problems emanate from the impact of the shadow on our ordinary waking consciousness. Our hidden desires, our envies, our bitterness or anger, when not fully understood, not brought fully into awareness, can influence our reactions; our behaviours; our attitudes; and our relationships. Parts of our personality that we would rather not acknowledge, like the spiteful child, or the angry bully, the trembling coward: parts that we do not like to acknowledge as they conflict with the view we have of ourselves. These parts dwell in the shadow, influencing us in ways that we do not quite understand. The shadow may also contain great resources, parts, or aspects that we fail to see or acknowledge, strengths, abilities or talents that may be hidden from us. The shadow is thus not a place of positivity or negativity, it is simply a place of the unseen.

Why is shadow work important / what can it do for you?
It is important because it raises the hidden into the light, the unknown into awareness. Whatever we do not understand can influence us in ways in which we are unaware. If I do not know I have a gift for music, I might spend a lifetime avoiding musical settings but not knowing why. I limit my choices in life without even understanding that I am doing it. If I am filled with rage but fear acknowledging it in case I lose control and become destructive, I might spend a lifetime avoiding conflict by avoiding close relationships or challenges in which the rage is stimulated.
By exploring the shadow, we bring the unknown into the known. When we bring forth knowledge and understanding we equally bring forth choice. We become more clear in the motivations for our actions and attitudes. A person who actively works on their shadow comes to know themselves more deeply and more fully. They become aware of the foibles, the limits, the hidden talents that they possess. There are less unpleasant surprises in life because the unconscious is less likely to arise spontaneously, and yet there is also much greater access to creativity and to exploration. Life becomes an adventure because there is nothing about oneself that you are unwilling to explore or to engage.

How does one do shadow work?
Shadow work is best done with a trained therapist. There are many self-help books and websites that can help develop an interest or curiosity, but because we are dealing with aspects of ourselves that remain hidden, it is best that the works at least begins with someone who is trained to help us see into this part of ourselves.
By therapeutic mirroring, the act of skilfully feeding back what is experienced and observed, by gentle amplification (the skill of developing and elucidating the unseen), we can quickly start to expand the cartography of our own minds. It is easier to enjoy a good bush walk with a clear map of the terrain, it is easier to relax into the environment if you know where you are going, so the guide in shadow work helps to map the terrain of the shadow.
As we become more skilled and understanding, we can explore more independently. There is never a complete end to the shadow just like there is no complete end to the known universe. What is different in well-supported shadow work, is the sense of adventure in the exploration. Fear recedes and is replaced by open curiosity; reactivity is replaced with choice.

Psychedelics and the Shadow
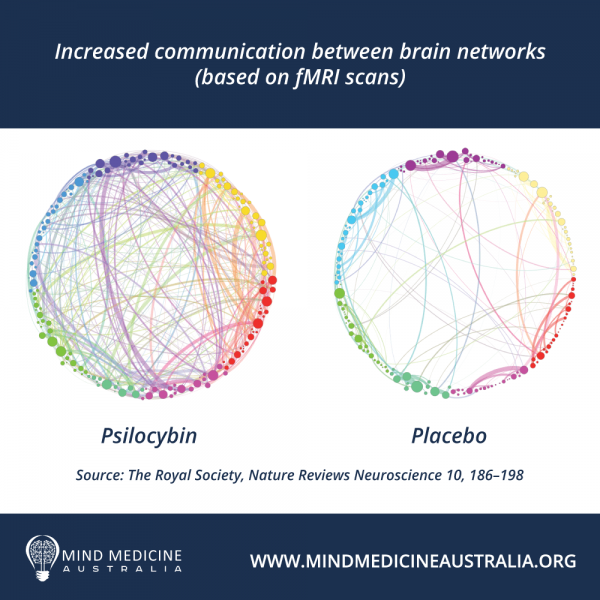
The use of psychedelics and empathogens is another way of accessing the Shadow. These medicines, in differing ways, reduce the rigidity of our ordinary waking consciousness and allow access to the wide and disparate contents of the mind beyond awareness: the Shadow. Material breaks through. Sometimes symbolic material, sometimes ancestral, sometimes personal, and biographical, sometimes existential. With the use of these medicines, we open to the vast extent of possibility.
The work then becomes the way in which we ground these new insights and experiences, the way in which we integrate them into the always changing affective narrative of self. This is a narrative that is not just a sequence of events, but events embedded in the felt sense: the highs and lows, the joys and sorrows, the love and the loss, the birth and death, the creativity and excitement of our always evolving story of who we are in this life. The content of the Shadow can be fascinating to us.
Effective integration supports our discrimination: it helps us draw upon those aspects of experience that can best help us improve our own lives and relationships through emotional stability, generosity, kindness, compassion, gratitude and connectedness. Without this skillful process of integration and discrimination, we run the risk of becoming lost in the multiplicity or possibilities contained within the Shadow.
You may have met people like this: slightly ungrounded, constantly searching for new experience but perhaps without being fully present. These people have access to the Shadow but are perhaps yet to learn to skillfully navigate it, instead they are buffeted by waves of emergence, unclear in which direction to walk.
Psychedelic-Assisted Therapy, when conducted by an appropriately trained and qualified clinician, can be a skillful means through which we can learn to move through the contents of the Shadow: navigating, discriminating, and integrating those aspects that can help one move beyond the constraints of suffering. These therapies can help one move into a new realm of possibility; towards a richer and more meaningful and more integrated affective narrative of self.
Nigel Denning
MA, MPsych
Nigel Denning is a Counselling Psychologist with 30 years of experience in the mental health sector. He is the Managing Director and co-founder of Integrative Psychology and the Mind Medicine Institute.
Nigel’s expertise covers developmental trauma, institutional abuse, family violence, attachment disorder, relationship therapy and advanced concentration meditation. He works with individuals, couples, families, groups and organisations. Nigel has been involved in therapy and court reporting on several hundred cases from the Royal Commission into Childhood Institutional Sexual Abuse. Nigel is a former Family Violence Coordinator for Relationships Australia. He has conducted research at the University of Melbourne, Faculty of Medicine, under the supervision of Professor Kelsey Hegarty on male perpetrator typologies. For over 10 years Nigel facilitated group psychotherapy for male perpetrators of family violence. Nigel is an expert in trauma.
Nigel has extensive experience with psychedelic work internationally. He began working with altered states of consciousness 35 years ago when he was introduced to Holotropic Breathwork through the guidance of Alf and Muriel Foote. Twenty-five years ago, Nigel began to work with Dr Stanislav Grof, one of the leading pioneers in the clinical application of psychedelics. Nigel co-founded the world’s first Spiritual Emergency Centre based on Grof’s work, in partnership with Tav Sparks, Director of Grof Transpersonal Training in North Carolina. He was also lucky to meet Dr Albert Hoffman at a workshop organised by Grof at HR Geiger’s Museum/Gallery in Gruyere Switzerland. Nigel has also trained with the Multidisciplinary Association of Psychedelic Studies (MAPS) and successfully completed their clinician qualification. Nigel is passionate about educating clinicians into the potential of non-ordinary state work when done ethically and skillfully.